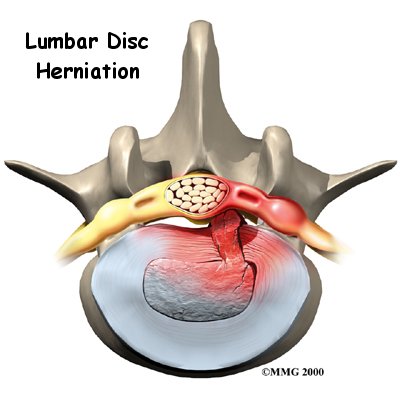
I cringe a little every time I hear a patient tell me that they have a slipped disc because the reality is that discs don’t slip. They may herniate, tear, prolapse, bulge or sequester,.. but slip? Never.
Sometimes doctors will use more simple terms to attempt to make things more understandable to patients, but when they use terms that give a totally wrong impression, I am not impressed. Sometimes patients come in with such strange ideas that the challenge of bringing them up to speed on what is really happening is a major undertaking. But, I digress…
When a patient says they have a slipped disc, I understand it to mean one of the above descriptors that are typically used on a radiology reports describing the findings of an MRI. But even though an MRI may show a herniation or bulge in a disc, the question that isn’t answered is, WHY? Why did the disc herniate? or more importantly, why isn’t the disc healing?
Every tissue in the body tries to heal itself. So when a disc is damaged, what I look for are the reasons that it is not healing. Some chronically damaged discs remain so because of activity (or more correctly, abnormal motion patterns), or because of inactivity. Some of the chronic disc problems are a combination of these. My job is to identify the causes and apply appropriate treatment.
An effective examination consists of various movements and motions coupled with muscular contractions or external support that feel better or worse which help me identify the why the problem persists. This way, I can address specific issues and get to the root of the problem… and hopefully explain it to the patient in a way that is understandable.
It has been said that ‘a person doesn’t care how much you know until they know how much you care.’ I try not to simply treat reported conditions or named diseases. Because of this, my practice model has long been one of identifying the causes related to your specific problem and treat the reasons it lingers.
Recent Comments