Following a car accident, many people wonder how serious their injuries are. Many also experience localized pain in the neck, lower back, or other areas, while many more will experience other neurologic symptoms such as radiating pain down the back of the leg or down an arm. True sciatica is felt when a person feels pain numbness or tingling down through a buttock and back of the leg. People ask, ”Can a car accident cause Sciatica?” Not only is the answer a resounding “Yes!,” But it is extremely important to understand what sciatica means for the health of your body.
You see, pain anywhere in the body is an indication of actual or potential damage to the cells and tissues of that region. Something must be done! In the case of nerve pain, it’s extremely important to discover the origin of that pain and take action to fix it. Sciatica is a term that means pain down the sciatic nerve. It is not a descriptor of origin or cause, but only a location and symptom. There are certain drugs that are very good at alleviating this kind of pain. But does that mean the origin of the problem has been fixed? Not likely. Most drugs invented for the reduction of pain are only for hiding or masking the pain. They do not promote healing. In fact, in the process of masking pain, this allows a person to do things they otherwise may not do because of the tissue damage that can progress if those body regions are able to move and function without pain. I have seen many people’s condition worsened by overusing a damaged limb, low back, or neck following a car accident because they were given such heavy narcotics, that they thought they were fine to go to work, engage in sports, and recreational activities. All the while, they felt fine in spite of the ongoing trauma that was occurring when using that body part.
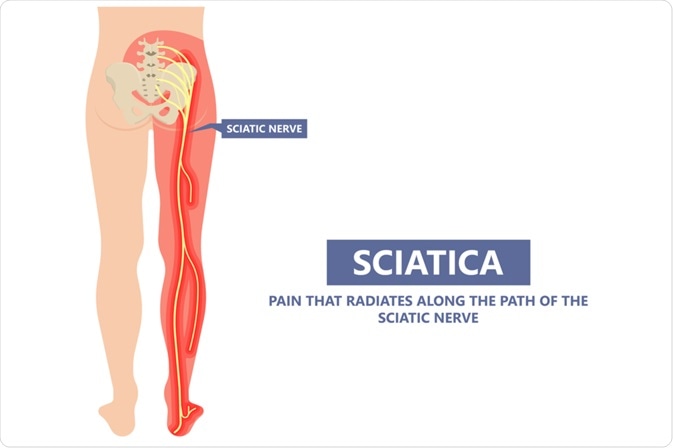
Sciatica Defined
Again, when considering the question, “Can a car accident cause sciatica?” The follow-up question should be “what does sciatica feel like?” Generally, sciatica is felt as pain it typically will originate in either one side of the lower back or top of the gluteal muscle. From there, sciatica can radiate through the lower gluteus area, down the back of the leg, even into the lower leg, ankle, and foot. Typically, a severe case of sciatica will feel like something akin to being stabbed in the butt with a red-hot poker from a fireplace. More mild cases may feel like pins and needles in the same region, or ants crawling up and down the back of the leg or tingling in the same region. These symptoms can typically be alleviated by changing the spine or lower extremity position. Some are so flared up and acute that finding a comfortable position is difficult. In the worst cases, over time, they may start to notice weakness in the leg. In the case of true sciatica, the strength loss will involve the inability to flex the knee, walk on the toes, or dorsiflex the ankle. The latter is called “foot drop.” These weaknesses indicate a very severe condition and it is imperative that is addressed immediately. If not resolved quickly, the patient risks permanent muscle weakness and/or paralysis.
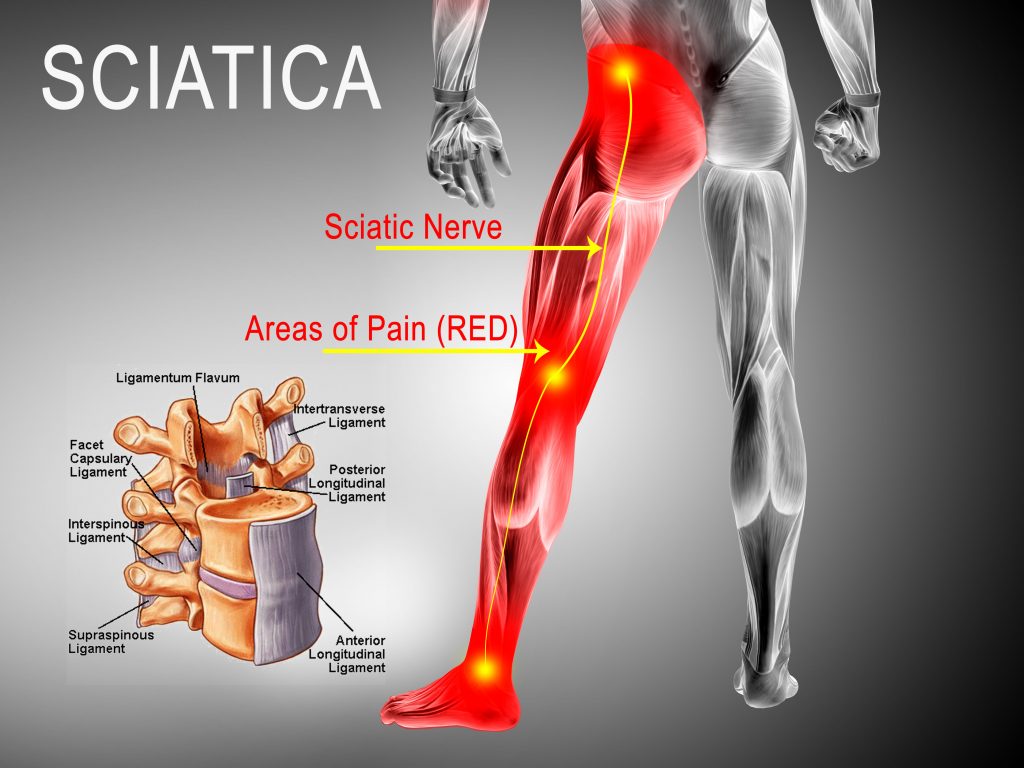
The sciatic nerve is the largest nerve in the body and is frequently injured in car accident injuries. A car accident chiropractor who specializes in these types of cases will look for the origin of sciatica and strive to affect the direct cause of that nerve impingement. Sometimes, sciatica can be a simple overstretch on the sciatic nerve. When you consider forces involved in a car accident, if a person is not wearing a seatbelt their body could be thrown in whiplash motion which would not only overstretch and tear muscles, ligaments, and tendons but can also put a great strain on the sciatic nerve, directly damaging it. Overstretched nerves, can take a long time to heal, and are best addressed by protecting the area with bracing or supports, resting, controlling the inflammation around the injury, and treating the surrounding regions which are likely injured at the same time. The thing to remember about the sciatic nerve is that it passes through many tissues in the course it runs down the leg. Inflamed muscles such as the piriformis and the hamstrings, can be a contributor to sciatic symptoms. And in the case of a car accident injury, these same muscles that surround the sciatic nerve, when damaged, can create adhesions to the nerve itself thus leaving a person with ongoing pain and symptoms indefinitely,… even after the tissues have “healed.”
Hidden Damage
It’s important to recognize that when tissues are overstretched, there is micro-tearing within the tissue which also means there is bleeding in that region to some extent. If you have ever suffered from a severe car accident injury, you may notice discoloration under the skin, much like a bruise, without ever hitting a body part on the interior of the vehicle. That bruising is an indication of torn tissues that are now trying to heal. The bleeding from torn tissues is damaging to cells and acts almost like a glue that damages nerves and muscles, this then leads to fibrotic adhesions, adhering one tissue to another. Nerves to muscles, muscles to other muscles, ligaments to tendons,… A whole cascade of painful scarring can be very problematic to a person’s recovery.
When we consider car accident injuries, typically neck is the most injured area. However, because of the structural differences between the spinal column in the neck and the lower back. The lower back is where the greater amount of disc herniations and bulges occur following a car accident injury, in my experience. Disc herniations, bulges, and protrusions are the most common causes of sciatica. In my practice, this accounts for approximately 35% of all conditions that I treat. Disc herniations come on for many reasons, everything from acute traumatic injury to poor posture. The most prevalent thing that all disc herniations have in common is the origin of spine flexion, either sudden and sharp or slow and steady.
Disc Damage: Sudden and Sharp vs. Slow and Steady
When you consider the anatomical makeup of a spinal disc, especially in the lower back or lumbar spine, you come to understand that the outer lining of each disc is a tough material referred to as the annulus. The center of the disc, or nucleus pulposus, is a very tough, viscous, gel-like material. The spinal vertebra above and below with the intervertebral disc in between, comprise a joint in the spine. These joints allow for flexion movements in various directions, in fact, all directions. In anatomical terms, flexion of the spine is referring specifically to forward bending. During forward bending, there is more pressure at the front of the annulus by the bones above and below than when standing neutral. The same goes for any motion such as side bending or extension (back bending). At the same time, more pressure on one area of the annulus will also cause a shift in pressure on the nucleus pulposus. Imagine a water balloon sitting between the two flat surfaces of the spinal bones. Now, when you flex the bones, the pressure on one side of the water balloon increases while the other side decreases. In normal movements, flexing the spine in various movements is not a problem. But now imagine very sharply flexing and extending the bones within less than 1/10 of one second. Now the risk of popping the water balloon is highly increased! This is what we notice in the case of car accident injuries,… when the low back is thrown suddenly and sharply forward and backward, compression and overstretch (or overstretch and compression) may cause a rupture or herniation in the intervertebral disc.
The other way that discs are damaged is the slow and steady reasons. These types of disc bulges or disc herniations come on over time with micro traumas such as poor posture (both seated and standing), poor bending and lifting habits, loss of core stability, or uncorrected movement disorders following a previous injury. All of these “microtraumas” can add up to, what seems like, a sudden event. When, in actuality, the disc(s) has been under stress for quite some time. It then only takes a “final straw” for someone to realize and feel that there was an underlying issue, to begin with. Many times people will come into my office indicating that they “threw their back out” when bending over to pick up a pencil off the floor. What they don’t realize is that there was already a significant disc issue, but since it wasn’t manifesting as pain, they think it’s the pencil’s fault.
Initially, the rapid disc injury may only feel like stiff muscles or a simple low back injury. This can be mostly true because the initial low back whiplash injury also overstretch is the muscles tendons and ligaments surrounding the same disc. All these areas typically will become inflamed immediately following the accident. Therefore the individual wakes up the next morning stiff and sore, calls the doctor, and is prescribed a simple muscle relaxant. These muscle relaxant drugs may give some amount of relief for the persons lower back pain, but end up not doing the disc any favors sense there is now disc damage in the form of a simple bulge, herniation, or protrusion of one or more of the discs in the lumbar spine.
Muscle Guarding
Whenever there is significant damage in the body, all muscles surrounding that damage will contract as a means to inhibit further damage by allowing that joint, or body region, to move unrestricted. An example of this that is easy for most people to understand is fractured. When someone breaks a bone, this muscle guarding or contraction of muscles surrounding the injury will stop further motion as the body’s way to protect the area. If this did not occur, the broken limb would easily be able to flop around while the shards of bone at the fracture site would be free to cause cuts and abrasions in surrounding tissues such as blood vessels, nerves, skin, muscles, and other connective tissues. The same is true for protruding discs, herniated discs, or bulging discs. In the case of a herniated disc, once the annulus of the disc is ruptured, too much movement in that area will cause further rupturing and protrusion of the nucleus pulposus (as described above), thus leading to greater injury and potential nerve impingement which causes sciatica and other nerve radiations depending on the spinal area in question. In the worst cases, as described above, the herniated disc may progress to a protruding disc that could be large enough to put pressure on the spinal cord and cause very serious conditions of loss of strength, muscle atrophy, bowel and bladder dysfunction, and even paralysis.
While treating muscle spasms is an important part of healing after a car accident injury, it is more vital to address the underlying cause, if any, for that muscle spasm and guarding in the first place. In the case of muscle guarding, once a fracture heals or once a disc herniation resolves, the treatment of the muscle spasms surrounding that area or muscle guarding protecting the region, will many times resolve on its own. However, the resolution of the remaining muscle spasms can be helped by a therapeutic intervention such as electrical muscle stimulation, therapeutic ultrasound, laser therapy, or trigger point injections.
Fixing Disc Herniations and therefore, Sciatica
Spinal disc decompression is a very effective way to resolve lower back pain and sciatica stemming from disc herniations, disc bulges, and disc protrusions. The research began nearly 30 years ago, in the 90s, regarding the notion of spinal decompression therapy as a way to mitigate discogenic pain stemming from disc bulges. In those days, a multidiscipline team of physicians began studying and working on this new idea of fixing disc herniations without surgery. Up until this time, whenever you heard the word “disc bulge,” the word “surgery” typically followed. I am happy to say that with my learning of spinal decompression, I have been able to literally save thousands of patients from having to undergo spinal surgery.
The process of spinal decompression therapy is the act of creating a vacuum, or negative intradiscal pressure, in order to bring the disc back into its normal configuration or shape. As I described earlier in this article, disc bulges, disc herniations, and disc protrusions all include damage to either the annulus (outer lining) of the disc or the annulus and nucleus pulposus (jelly center). The act of creating this “vacuum” effect is performed during a variable weighted negative axial pressure applied to the spine. This works quite effectively for necks (cervical spine) and low backs (lumbar spine). In doing so, discs now have a better chance of healing especially with the application of therapeutic laser. In my clinic, we always use the laser in conjunction with spinal decompression. The net effect of these two therapies together is highly effective in resolving sciatica, stemming from lumbar spine disc issues.
In addressing sciatica that has resulted from a car accident injury, I am always careful to be sure to address all surrounding structures in order to fully restore the injured area to a state of pre-accident status. This means checking all tissues that may be involved in any way to cause sciatica pain resulting from an automobile accident. After we have fixed the disc issue, we address the muscle spasms of the area with electrical muscle stimulation, ultrasound therapy, deep tissue massage, or other therapeutic intervention to give relief. Homework given to a patient may involve ”nerve flossing” or other stretching techniques of muscles, ligaments, and tendons that are potentially impeding sciatic nerve function.
With over 20 years of experience in treating car accident injuries and the resultant disc herniations and sciatica, I am confident in my abilities to both diagnose and treat all sciatic conditions stemming from these types of injuries. Please don’t take this to mean that I can fix every single patient that comes into my office. This is not the case. When necessary, I will refer to spinal surgeons for the few cases that are unresponsive to spinal decompression. But, with 95% effectiveness in treating sciatica and accompanying disc protrusions, disc herniations, and disc bulges, I feel that my methods are certainly worth trying prior to going under the knife.

Recent Comments